Liver Diseases

What is liver?
Liver is an organ, which is around 1.2 kg in an adult situated on the top right quadrant of the abdomen.

What does liver do?
Liver is an important organ. Blood from stomach and intestine passes through liver , where liver extracts
Read More
nutrients from the blood and produces protein, sugar, fat etc necessary for growth and development of body. It produces substance that helps in blood clotting. It also removes drugs and toxins from blood and cleans it. It has also got immune function and protects us from harmful pathogens.

What causes Liver disease?
Inborn errors of metabolism, anatomical malformations of liver, bacterial and viral infection, tumours etc can cause liver disease.

How does children liver disease differ from adults?
Usually children are born with liver disease, which could manifest ever after few days while most of the adult disorders are aquired.
Jaundice in Newborn: Act Swiftly
Jaundice, which persists after two weeks in term babies and three weeks in preterm babes, is pathological and requires further investigation. Apart from blood group incompatablity( rhesus & ABO), lot of anatomical and functional disorders of liver could cause jaudice during neonatal period. Anatomical disorers such as biliary atresia, cysts etc, hereditary disorders such as Progressive Familial Intrahepatic cholestasis (PFIC), Alagile etc and metabolic problems such as galctosemia , tyrosenemia could cause jaundice during neonatal period.
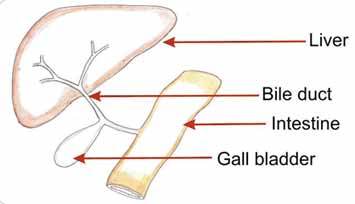
Biliary Atresia
Biliary atresia is a condition where the bile ducts( tubes draining bile from liver to intestine) are blocked or absent. It is of utmost importance to diagnose this condition early, so that surgical treatment could be initiated. Over half of infants undergoing surgical treatment (portoenterostomy) for biliay atresia with in first 2-3 months will clear the jaundice and have a greater than 80% chance of a good quality of life, reaching adolescence without liver transplantation. Baby’s urine is colorless, if there is dark urine along with suspected pale stools (see chart) , consult your pediatrician urgently
Normal
Biliary Atresia
Metabolic Disorder in Children
Metabolic disorders in children: What is it?
Our food consists of various carbohydrates, proteins and fats. When we consume them they get digested in stomach and get absorbed from intestine. From intestine, blood carries these particles into liver. They are further broken down to simple sugars, aminoacids and fatty acids/ cholesterol. During the breaking process energy is created in the form of heat (this is how body is warm). Using these basic particles of simple sugars, aminoacids and fatty acids/ cholesterol, the liver cells manufacture complex sugars, proteins and fats necessary for growth and development of our body. For breaking and re synthesising our body depends on enzymes. In the absence of enzymes, the process of breaking and re synthesising is defective and not complete resulting in diseases, called metabolic disorder.
How many metabolic disorders are there?
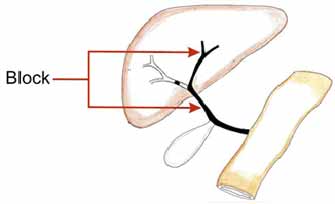
There are more than 100 types of proteins, sugars and fats and there are 100s steps involved in gradual breakdown to re-synthesis. So there are 1000s of enzymes in the body. Absence of any one enzyme would lead on to block in the pathway resulting accumulation of toxic by products which could damage liver, kidney, brain etc. So there are hundreds of metabolic disorders of which some are very common and some are very rare. In simple terms, metabolic disorder is a broader term, which encompass hundreds of specific disorders.
Could you give a simple example?
When protein is broken down ammonia is produced, this ammonia is very toxic to brain cells and liver convert this ammonia to urea, which is easily excreted in urine. This process of converting ammonia to urea is called urea cycle and has five steps mediated by 5 enzymes. Absence of even one of the enzyme, could lead to increased ammonia in body, which will affect brain cells and eventually cause death.
What is the clinical manifestation of metabolic disorders?
They can manifest in various ways. Affected patients can have low blood sugars, jaundice, renal failure, liver failure, fits, behavioural changes, sometimes coma and death.
When do they manifest disease?
The metabolic disease manifest only when they eat the specific sugar, protein or fat, for which they lack enzymes to digest. Sometimes, other metabolic pathways could compensate or remove the toxins and the disease manifests only during periods of stress like prolonged fasting or infection.
Why it affects children more?
Children are born with the disease as it is hereditary condition, but manifestation happens only when that specific food component is introduced. So potentially the disease manifestation can happen at any age. For example there is a disorder called Hereditary Fructose Intolerance, where the patient cannot digest fructose (type of sugar found in fruits and vegetables). So disease manifests at diarrhoea or liver failure, only when fruit and vegetables are introduced in to their diet. This usually happens around 7 or 8 months, when parents introduce fruits to baby.
How common is metabolic disease?
The incidence of disease varies from 1 in 2500 to 1 in several million. Few disorders are so rare that, only four of five cases have been reported worldwide.
I am scared whether my child has got it, when should I think about it?
There are few signs and symptoms that suggest underlying metabolic disorders. Frequent low blood sugar levels leading on to fits, delayed developmental milestones, jaundice, enlarged liver or spleen, generalised muscle weakness (hypotonia) are few of common symptoms related to metabolic disorder.
Can it be prevented?
Usually they are hereditary disorders, where both mother and father pass on the genes. We call them carriers as they have one defective gene and one normal gene and don’t manifest disease. When they have a child there is one in four chance that the defective genes could come together and cause disease (in theory one in four children are affected if both parents are carriers). This is why doctors discourage marriage with in relatives.
Can it be diagnosed immediately after birth?
There are screening test available for common metabolic disorders, usually it requires only a drop of blood on filter paper from newborn baby. Number of metabolic tests carried out varies from country to country, depending on common metabolic disorders present in the country.
How it could be treated?
Dietetic management forms the basis of treatment. Exclusion of the specific sugar, protein or fat is the only treatment. As children needs all the three components in their diet for growth, it is very difficult to manage. There are special feeds available in the market but still it might be difficult to eliminate certain food components. There are certain medicines, which will help eliminate the toxins from body, but they work only partially.
Once diagnosed can it be cured?
It depends on where the enzyme is present predominantly. Most of the enzymes are present predominantly in liver and liver transplantation offers cure to many metabolic conditions. If the enzymes deficiency is all over the body, no effective treatment is available, apart from dietetic restriction.
What’s the future?
Research is underway to develop the missing enzymes so that it could be injected (like insulin), but there is a long way to go.
Acute liver failure
The liver could fail suddenly in previously well child, resulting in jaundice and synthetic failure. The cause could be due to infection, metabolic liver conditions, autoimmune disease etc. In around 30 to 40% of cases the even after exhaustive investigations the diagnosis could not be found out. This disease progresses rapidly and could cause death in few days time, unless treated appropriately. Conditions like Wilson’s disease, autoimmune liver disorder often fails to respond to medical management and require liver transplantation. Metabolic liver disease usually gets better with dietetic restriction. It is essential to find the underlying cause of liver failure to plan the type of liver transplantation. Auxiliary liver transplant, where a portion of donor liver is placed alongside of the native liver, could be done in liver failure due to hepatitis A, Hepatitis E etc. Once the acute insult is over the native liver regenerates and immunosuppression could be stopped, so that transplanted liver atrophies and the patient can live with their own liver.
Alagille syndrome
Alagille syndrome is a multisystem, genetic disorder. It is classically described as the constellation of characteristic facies (triangular face, broad forehead, pointed chin), cholestatic liver disease, cardiovascular anomalies (most commonly peripheral pulmonic stenosis), ocular abnormalities (posterior embryotoxon) and vertebral anomalies (commonly butterfly vertebrae). The liver disease could vary from mild symptomatic itching to severe jaundice and liver failure. Mild liver disease could be treated medically but severe liver disease could warrant liver transplantation.
Caroli’s disease
This is a condition where there are multiple cysts in the liver which could get infected and cause sepsis. Some newborn infants with severe autosomal-recessive polycystic kidney disease have extensive cystic bile duct changes, but renal insufficiency dominates the clinical picture. Ultrasound of the liver is often adequate for diagnosing Caroli disease; cholangiography is confirmatory. The outcome is related to the severity of renal disease, and/or the development of liver infection and fibrosis with portal hypertension.
Progressive familial intrahepatic cholestasis in children (PFIC)
Progressive familial intrahepatic cholestasis is a group of inherited disorders, which is common in India. Infants presenting with mild to severe jaundice, low GGT, elevated serum bile acids, failure to thrive and severe itching. There are three types of this disease and it could affect intestines and cause chronic diarrhoea. With mild itching these condition could be managed with medication, but in severe form of disease, “ biliary diversion” surgery could be done. In this surgery the bile is diverted either externally or internally, so that total bile acid pool is depleted, resulting in decrease of jaundice and itching. In severe cases with cirrhosis and liver failure, liver transplantation is the only option. This condition increases the risk of liver cancer in children and so these children require constant surveillance.
Non-alcoholic Fatty liver disease (NAFLD) in children
With fast growing economy, our country faces a new type of malnutrition in children, obesity. Fat deposition in liver and progression to liver cirrhosis is common in people who consume large amount of alcohol. Over end of last two decades fatty liver is being increasingly seen in children on routine ultrasound, particularly in obese children. People are aware of obesity and its complication in adults but when it comes to children, they don’t take it as a health problem. Similar to adults, children could also develop complication either during childhood itself or in their teen age due to obesity. With lot of eat outs serving fried foods and pizzas stuffed with calories and fats, prevalence of fatty liver disease is increasing in India. At present, the general prevalence of paediatric NAFLD is estimated at around 3-10 % in normal weight children, whereas this increases up to 50-70 % in obese children. The management consists of life style modification, increase in physical activities and appropriate dietetic management. The disease could gradually damage the liver and progress to liver cirrhosis requiring liver transplantation.

 العربية
العربية English
English